
Patients and age/sex-matched controls were young and most often male ( table 1). Patients with narcolepsy/hypocretin deficiency have increased BMI and a tendency for increased sleep-disordered breathing Δ V′ E/δ S p,O 2 and δ V′ E/δ P CO 2 values were analysed both with and without correction by body surface area (BSA), so as to adjust to size differences due to the range among subjects. V′ E was regressed linearly against the carbon dioxide tension ( P CO 2) values (hypercapnic testing) or against the fall in S p,O 2 from 90% (hypoxic testing), and responsiveness reported as the slope of the linear regression: δ V′ E/δ P CO 2 and δ V′ E/δ S p,O 2, respectively. Hypoxic testing was concluded when oxygen saturation neared 70%. This set-up resulted in a falling end-tidal CO 2 value as ventilation increased. Hypoxic testing was performed using an anaesthesiology rebreathing circuit, with a carbon dioxide (CO 2) absorbent, placed on the inspiratory line. Patients were in the seated posture connected to the circuit, wearing a facemask. Responses to progressive hyperoxic hypercapnia were assessed using the rebreathing technique of Read 19. The studies were performed at 10:00–12:00 h. In the (unlikely) event that patients or healthy subjects were taking drugs known to affect the MSLT, recordings of the PSG or MSLT and ventilatory testing were performed without these medications for ≥15 days. Sleep stages of both PSG and MSLT were scored in 30-s epochs following the Rechtschaffen and Kales 18 criteria.
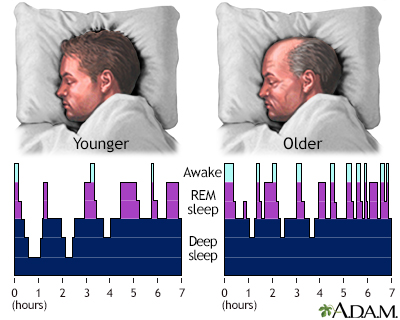
The REM sleep latency was defined as the time from the beginning of sleep onset to the first epoch of REM sleep. The sleep latency was defined as the elapsed time from lights-out to the first epoch scored as sleep. The MSLT was performed to determine sleep latency and probe for the presence of sleep onset REM sleep (SOREM). Mean S p,O 2 and lowest S p,O 2 during sleep were also calculated. The AHI was calculated as the number of apnoeas and hypopnoeas per hour of total sleep time, and further examined as per hour of rapid eye movement (REM) and non-REM time. The absence of airflow in the upper airway with and without ribcage and abdominal movement was defined as obstructive sleep apnoea and central sleep apnoea (CSA), respectively in a mixed sleep apnoea (MSA), there were features of both central and obstructive apnoeas/hypopnoeas in the same event. An apnoea was defined as the cessation of airflow at the nose and mouth lasting for ≥10 s, and hypopnoea was defined as a decrease in airflow, ribcage excursion or abdominal excursion by >50%, which was associated with an oxygen desaturation of ≥4% below the preceding baseline or with an arousal. The overnight recording included electroencephalogram (EEG) (C3/A2 and C4/A1), chin electromyography, anterior tibialis electromyography, microphone recording for snoring, electro-oculography, ECG, nasal–oral airflow, thoracic and abdominal effort, and arterial oxygen saturation measured by pulse oximetry ( S p,O 2). Overnight nocturnal PSG was followed by MSLT the next day. Results indicate an unexpected finding that the mechanism for differences between patients and controls in hypoxic responsiveness could relate to HLA marker status, rather than disease. Patients had depressed hypoxic responsiveness (0.13☐.09 versus 0.19☐.13 L Despite similar spirometric values, patients had a higher apnoea/hypopnoea index (AHI) (2.8±5.4 versus 0.8☑.6 h −1 p = 0.03) and lower minimal oxygen saturation during sleep (87%☗ versus 91±4% p = 0.0002), independent of age, sex and body mass index. All patients and 49% of controls underwent polysomnography and multiple sleep latency testing. Hypocretin deficiency was determined either by measures of cerebrospinal fluid hypocretin-1 (37 patients) or by positive HLA-DQB1*0602 status. min −1 per % S p,O 2) responsiveness, and by spirometry.mmHg −1) and hypoxic (δ V′ E /change in arterial oxygen saturation measured by probe oximetry (δ S p,O 2) L.130 patients with narcolepsy–cataplexy (mean± sd age 20☑0 yrs, 69% male) and 117 controls (22☖.9 yrs, 62% male) were recruited and tested for human leukocyte antigen (HLA)-DQB1*0602 status, hyperoxia hypercapnic (change in minute ventilation (δ V′ E)/carbon dioxide tension (δ P CO 2) L We hypothesised that hypocretin (orexin) plays a role in the determination of ventilatory chemosensitivity.


 0 kommentar(er)
0 kommentar(er)
